22:29 (IST)
The last session in this evening's conference – a session on vaccines and public health policy – is now a go.
22:28 (IST)
For mental health treatments, there's a lot of evidence-based therapies that have been proven to work. We need to be able to take some risks and accept what might seem unconventional – whether it's billboards or a game app that uses a methodology rooted in psychology – to address the needs of the people seeing mental issues as a result of COVID-19, says Dr Homes suggests.
22:25 (IST)
One of the biggest takeaways is to adapt the public health care system is to fit the needs of the patients. Right now, while we're ready to treat patients, patients aren't necessarily presenting themselves for care. And we need to be able to think of how to care for the wide range of patients, based on the needs and behaviour of patients, to serve them better, Dr Russman says.
22:20 (IST)
Some of the new groups we're seeing mental health issues in are COVID-19 patients in the ICU, and frontline health workers, who are at risk of traumatic stress disorders like PTSD. It's important we incorporate solutions, like public health messaging, are important additions in public health systems. After all, mental health is very treatable, Dr Holmes adds.
22:18 (IST)
We're seeing that COVID-19 definitely affects mental health – what a pandemic can do affects us both in physical and mental levels. Vulnerable groups, like those already seeing mental health issues both minor and major, are being pushed further into distress. Anxiety is one of the most common illness we're seeing affecting different ages, from children to older adults, Dr Holmes says.
22:15 (IST)
The next segment is on the how COVID-19 has effected mental health and psychology, by Professor Emily Holmes, Distinguished Professor, Uppsala University.
22:14 (IST)
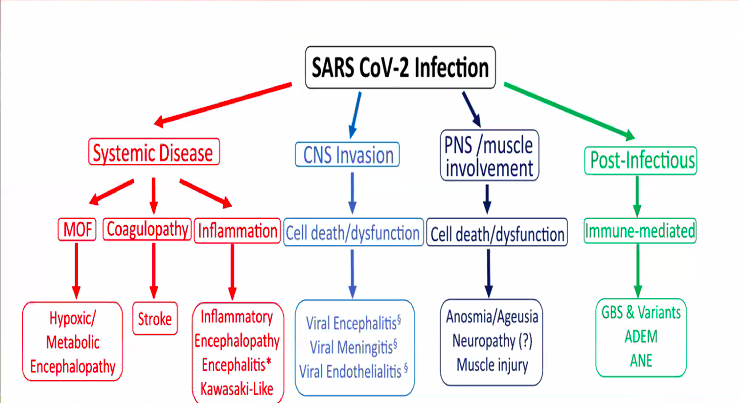
Over the last 6 months, we've learned that neurological symptoms are definitely seen in COVID-19 patients. Early diagnosis, and differential diagnosis will make all the difference in treating these symptoms, Dr Manji summarised.
22:13 (IST)
Dr Haji explains the four distinct ways in which COVID-19 patients showed complications in the nervous system and brain.
22:10 (IST)
The webinar has moved to the section discussing the effects and complications of COVID-19 in the brain. The speaker is Dr Hadi Manji, Consultant Neurologist and Honorary Senior Lecturer, National Hospital for Neurology.
22:08 (IST)
We're always innovating when it comes to addressing COVID-19 treatment. Daily meetings to discuss symptoms, the latest medical research to treat these symptoms, and bringing in international expertise and consultations have all been very useful in maintaining good quality healthcare considering the fast-evolving state of COVID-19 and medical research, Dr Russman concludes.
22:04 (IST)
Telemedicine has been another boon to care for stroke patients – it has reduced the number of staff needed to examine COVID-19 patients, without reducing the quality of care given, Dr Russman adds.
22:02 (IST)
When we were under a stay-at-home situation at the start of the pandemic, there were a lot fewer patients presenting symptoms, and sooner. Now, the cases are on the rise, but the trend we're seeing is that the symptoms are also presenting themselves later in the infection process than before. This makes it a little more risky for hospital staff, and requires ER staff need to be vigilant, and better equipped with protective gear, says Dr Andrew Russman.
21:57 (IST)
With those comments, the third session is now underway, hosted by the President of the Royal Society of Medicine. [He insists you tag any tweets you send out about the conference with the right hashtag...but only if you're saying nice things.]
21:52 (IST)
In all epidemic outbreaks, it's often those with comorbid conditions, older population and serious health conditions are ones to suffer most severely. The lesson to the health system is to attend aggressively to the most common comorbid conditions during non-epidemic periods too – diabetes, hypertension and obesity being some examples from India, says Prof Srinath.
21:50 (IST)
Diabetes and obesity are two of the most important comorbid conditions, based on the data we've seen, experts say.
21:48 (IST)
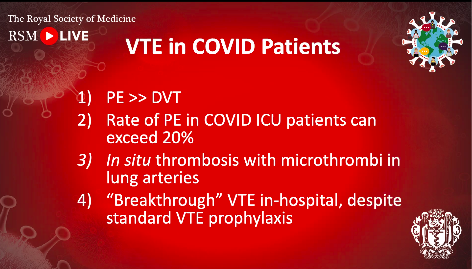
We know the infection begins 4-5 days before the onset of symptoms. If we know in advance who is more at risk, the symptoms of thrombosis (blood clotting disorder) can be better controlled using early-intervention and medicines like anti-coagulants or heparin.
21:46 (IST)
Meanwhile, here's a look at a summary screenshot from the thrombosis section.
21:41 (IST)
Sorry everyone, we're pretty adept with basic biology and medicine but the next section on thrombosis is going right over our heads :(
We'll be sure to send you time stamps at the end of our liveblog to the recording, so you can tune in and catch up on the findings from the sections on thrombosis if it's important to you.
21:34 (IST)
The focus on telemedicine during the pandemic could be a positive change that could stick with the Indian health system even after the pandemic isn't in play, Professor Srinath says.
21:33 (IST)
However, comorbid conditions are ample in the population, with urban diabetes, obesity and hypertension being the most prevalent. Among the people admitted with COVID-19, there have many cases of stroke, myocardial infarction have been commonly seen. There has been a sharp drop in the number of elective heart surgeries by patients, but there is still some data being gathered to assess why this is.
21:30 (IST)
In India, there has been a relatively low mortality rate, possibly due to the younger age profile of the country, says Professor K Srinath Reddy, Public Health Foundation of India.
21:28 (IST)
Effect of COVID on cardiovascular disease isn't a direct one, based on a lot of data from research in multiple nations including the UK. Many studies have reported fewer cases of mortality and admissions over the course of the pandemic, in heart patients that have experienced STEMI (ST-Elevation Myocardial Infarction), a serious form of heart attack observed in comorbid heart patients.
21:22 (IST)
The second panel on how COVID-19 has affected cardiovascular health in its patients kicks off. Experts will discuss some specific comorbities, in those with exisiting heart conditions, and how the health system has responded to address them.
21:20 (IST)
The pandemic can create a lot of damage, not just economically. The last great pandemic, the Spanish Flu, was quickly followed by the Great Depression, and extremism. The differences that continued afterwards culminated in a World War. In the case of COVID-19, the research community, the health community and the pharmaceutical industry and leading the way to find a solution. The world's shared goal towards a vaccine give me optimism that we won't see the same fate, Dr Kandor concluded, ending his welcome address.
21:16 (IST)
Whether we stand in the abyss or move to our mutual future depends on how we collaborate and coordinate our efforts, he says. COVID-19 has aggravated some already worrying problems, including and especially racism and other forms of discrimination.
"Progress is so much faster when national interests are set aside, and commercial interests are shelved for the greater good," Dr Kantor adds.
21:13 (IST)
As the first panel on respiratory effects ends, Dr Viatcheslav Moshe Kantor from the Kantor Charitable Foundation gives his Welcome Address (a technical blip preventing him from doing so at the start of the webinar). He thanks all the health workers at the frontline of the pandemic.
21:10 (IST)
Health experts and researchers have seen success in treating hypoxia with the use of pulmonary shunts. High-flow oxygen therapy and continuous positive airway pressure therapy (CPAP), which are less invasive methods, allow for more flow of oxygen with some artiificial assistance, and has shown a lot of promise in COVID-19 patients with severe respiratory symptoms.
30-50% of cases that see hypoxia don't need invasive methods/intubation to treat hypoxia, experts say.
21:00 (IST)
In Barcelona, where there's a mild second wave currently underway, one of the key challenges to preventing new cases is adequate physical distancing. This is a similar situation that many countries are in right now, with the opening up of lockdown restrictions, and the younger section of society feeling open to moving around in public spaces.
20:56 (IST)
In the UK, early collaboration from medical personnel across disciples – pulmonologists, cardiologists, anaesthesiologist and seniors physicians among others – helped bring different perspectives on the same issue, which helped prepare hospitals under the NHS to prepare for the unfolding pandemic.
20:52 (IST)
In small US cities like Rochestor, around 30% of the COVID-10 cases were affecting non-white Caucasians, which pointed to some sociological factors or specific biological factors rooted in race-specific differences fairly early on.
20:48 (IST)
A lot of these pre-surge measures in New York involved in increasing capacity and training in COVID-19-specific diagnosis and treatment. A lot of medical equipment including ventilators, ICU facilities, PPE, and increasing the number of beds were some of the first measures put in place.
20:46 (IST)
Experts are now sharing some key pre-surge measures that were put in place in New York, Barcelona and Minnesota took before cases began to climb steeply.
20:43 (IST)
The symptoms, especially ones that concerned the lungs, were different in COVID-19 that previous similar infections like acute respiratory syndrome (ARS).
20:42 (IST)
The pandemic began with a surge in cases in Wuhan, China. In a Feb 2020 dialogue with physicians in Wuhan, health experts were given key information that pointed to steroids being a useful therapy to treat COVID-19.
20:40 (IST)
The first session is now underway, with experts discussing respiratory effects, critical care and ventilator use in patients. The session is moderated by Dr Charles Powell. Speaking will be Professor Anita Simonds, Dr Richard Oeckler, Dr Eva Polverino.
20:31 (IST)
If you haven't registered yet, there's only a few minutes before the webinar begins. Head here to register and watch along.
20:30 (IST)
He'll be joined by some of leading experts in global medicine:
- Rt Hon Professor Lord Kakkar, Professor of Surgery at University College London
- Professor Anita Simonds, Consultant in Respiratory and Sleep Medicine at NHS Foundation Trust
- Dr Charles Powell, Janice and Coleman Rabin Professor of Medicine Systems and Chief, Division of Pulmonary, Critical Care, and Sleep Medicine at Mount Sinai Health System
- Dr Eva Polverino, Pulmonologist and Senior Investigator in respiratory infections at Vall d'Hebron Hospital, Barcelona; Chair for the Respiratory Infections Assembly at the European Respiratory Society
- Dr Richard Oeckler, Director, Medical Intensive Care Unit; Medical Director, Post-Intensive Care Syndrome Clinic; Consultant, Division of Pulmonary and Critical Care Medicine at Mayo Clinic
- Professor Barbara Casadei, President of the European Society of Cardiology and British Heart Foundation; Professor of Cardiovascular Medicine at University of Oxford, John Radcliffe Hospital
- Professor Samuel Goldhaber, Associate Chief and Clinical Director of the Division of Cardiovascular Medicine; Head, Vascular Medicine Section; Director, Thrombosis Research Group; Professor of Medicine at Harvard Medical School
- Dr Hadi Manji, Consultant Neurologist and Honorary Senior Lecturer at National Hospital for Neurology, London
- Dr Andrew Russman, Head, Stroke Program; Medical Director, Comprehensive Stroke Center at Cleveland Clinic
- Professor Emily A Holmes, Distinguished Professor, Department of Psychology, Uppsala University and Karolinska Institutet, Sweden
- Dr Andrew Badley, HH Sheikh Khalifa Bin Zayed Al-Nahyan Professor of Infectious Diseases and Enterprise Chair, Department of Molecular Medicine, Director, HIV Immunology Lab and Chair, Mayo Clinic SARS-CoV2/ COVID-19 Research Task Force, Mayo Clinic, Rochester
- Dr Monica Musenero, Assistant Commissioner, Epidemiology and Surveillance at Ministry of Health, Uganda
- Professor Robin Shattock, Professor of Mucosal Infection and Immunity, Imperial College London
- Professor Sian Griffiths, Emeritus Professor at CUHK; Advisory Member of the Board of Public Health England; Chair, Global Health Committee; Visiting Professor, Imperial College London
- Professor Sir Simon Wessely, Royal Society of Medicine President; Professor of Psychological Medicine, Institute of Psychiatry, Psychology & Neuroscience, King’s College London; Consultant Psychiatrist, King’s College Hospital and the Maudsley Hospital
- Professor Roger Kirby, Royal Society of Medicine President-Elect and Trustee
20:25 (IST)
We're pretty happy to see some Indian representation at the conference today, from Professor K Srinath Reddy, President of the Public Health Foundation of India.
20:19 (IST)
Hello all!
The conference hosted by the Royal Society of Medicine today is one of the first international health dialogues open to the public.
It brings in experts from medicine, health policy, academia, public health and psychology under one roof to discuss how the coronavirus pandemic has affected health. It will also conclude with a discussion on how best to avoid future pandemics from creating the level of devastation, and overwhelming health systems in nearly every country, the way the ongoing pandemic has.
The Royal Society of Medicine will be bringing together a group of thought leaders from around the world to share learnings and consensus on some key aspects of the COVID-19 pandemic and its impact on human health.
The webinar began at 8.30 pm IST, and is being streamed via the Royal Society's official website for registered viewers.
Leading health experts, as per the event website, will be part of discussions on the coronavirus pandemic, under four key areas:
- Respiratory effects: critical care and ventilation
- Cardiovascular complications and the role of thrombosis
- Impacts on the brain and the nervous systems
- Looking forward: research, vaccines and future management strategies
Experts will share the most effective ways to treat COVID-19 based on research and experience from around the world, and how the pandemic has affected the physical and mental health of patients. Also on the agenda is advice to improve treatment plans and strategies to lessen the impact of pandemics in future outbreaks.
https://ift.tt/3hKP5GR from Firstpost World Latest News https://ift.tt/2D7EHdg


0 Comments